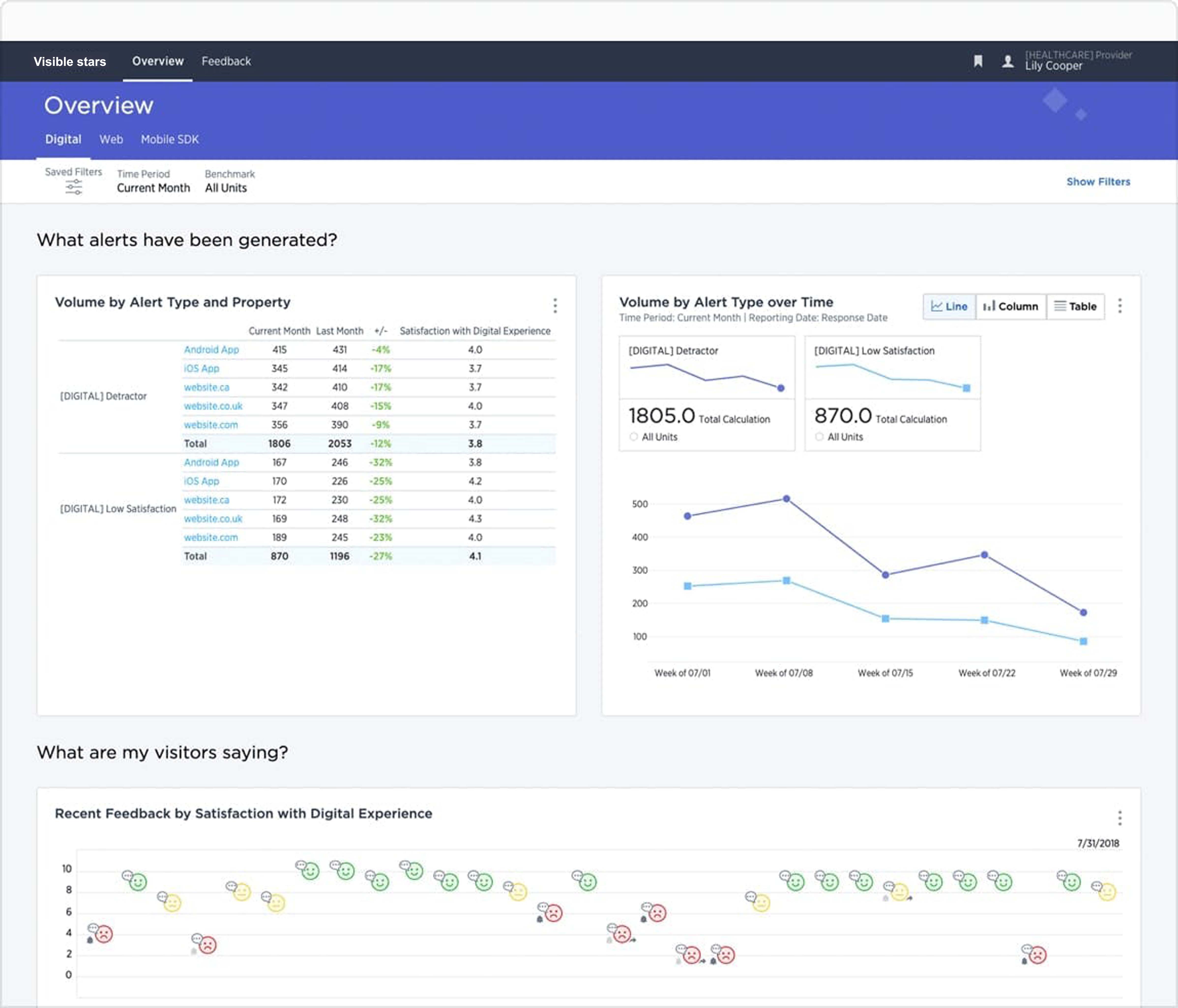
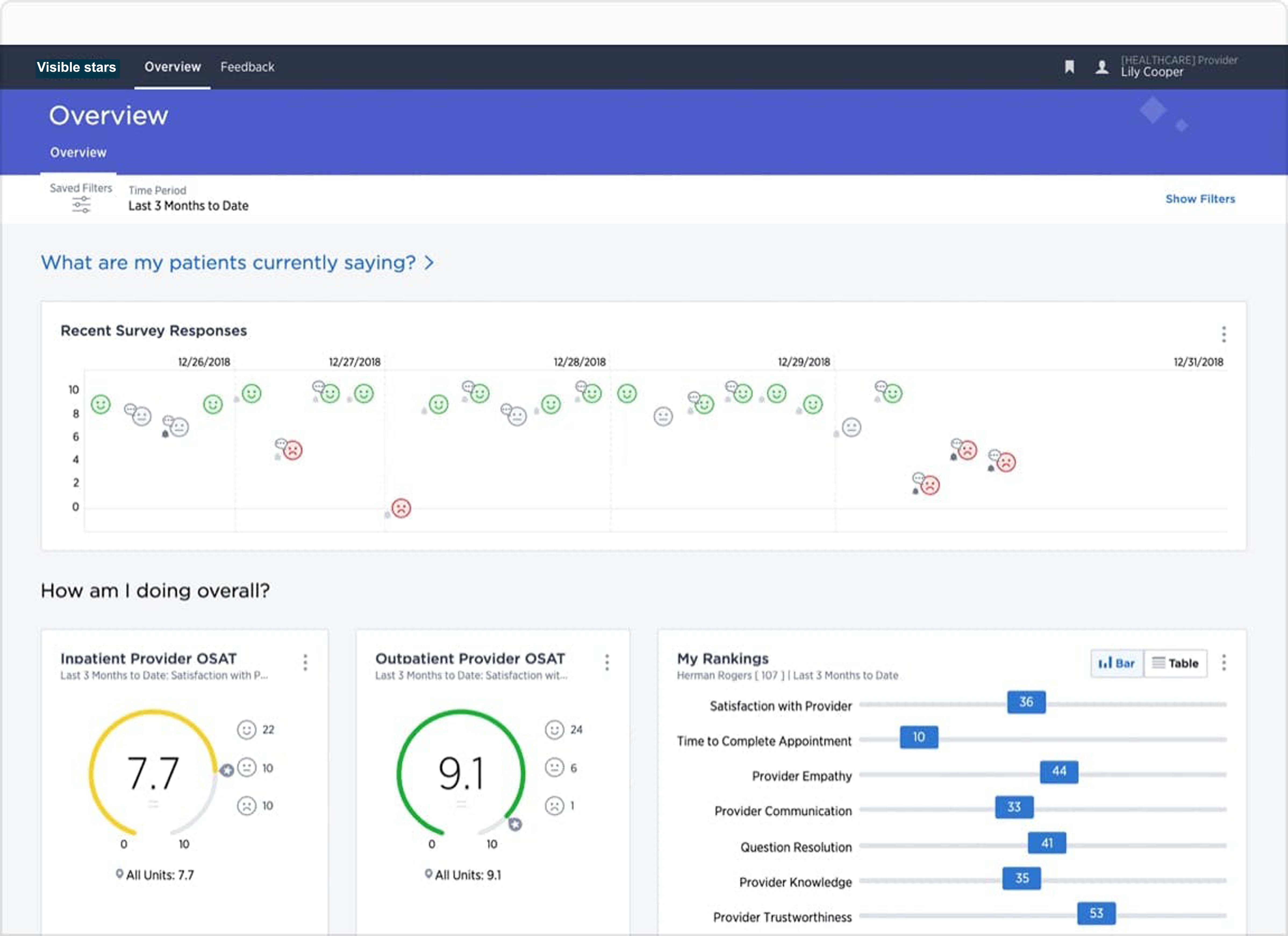
- Collect real-time signals across the patient journey and enrich with data from EHR and CRM systems for a holistic view of the patient
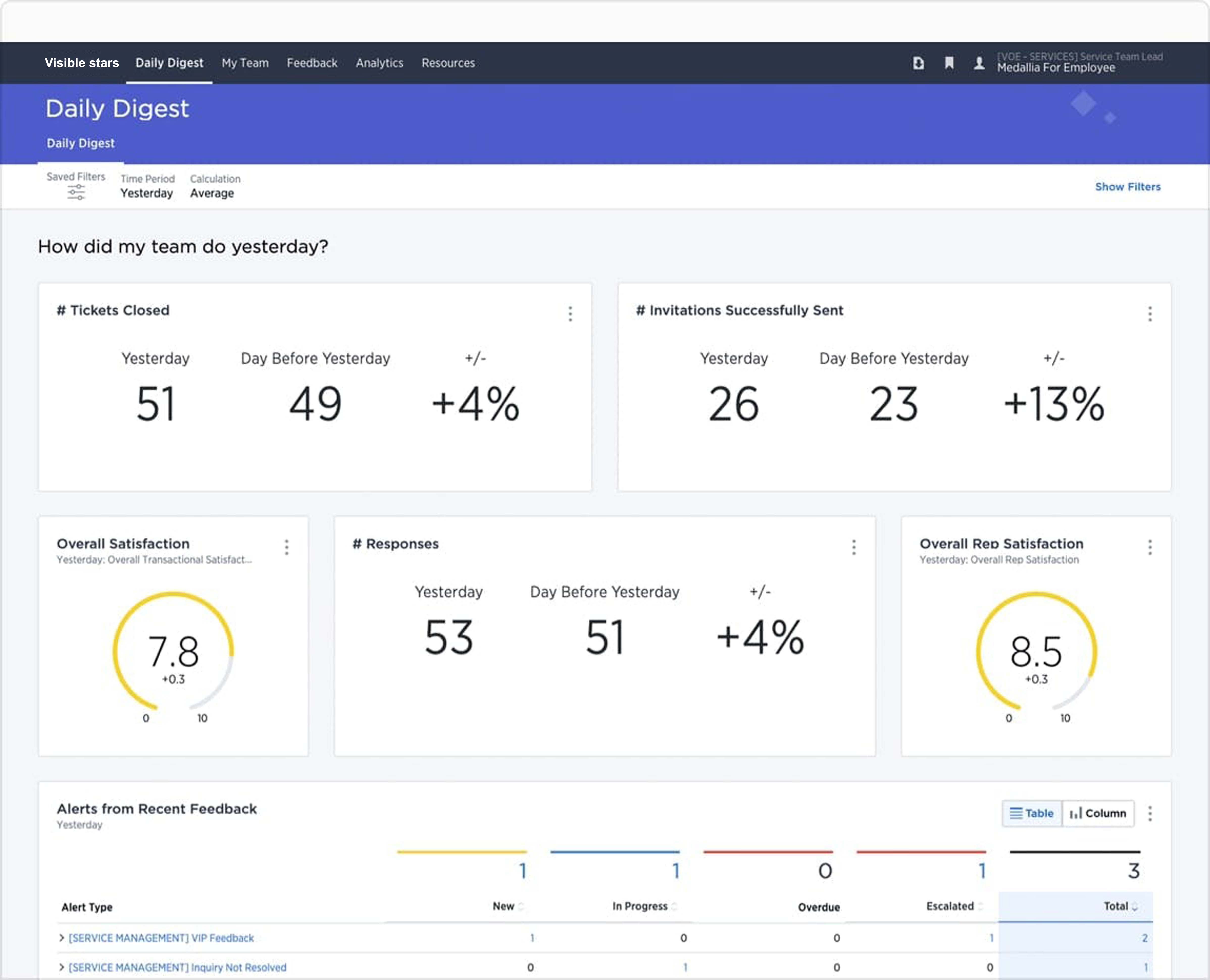
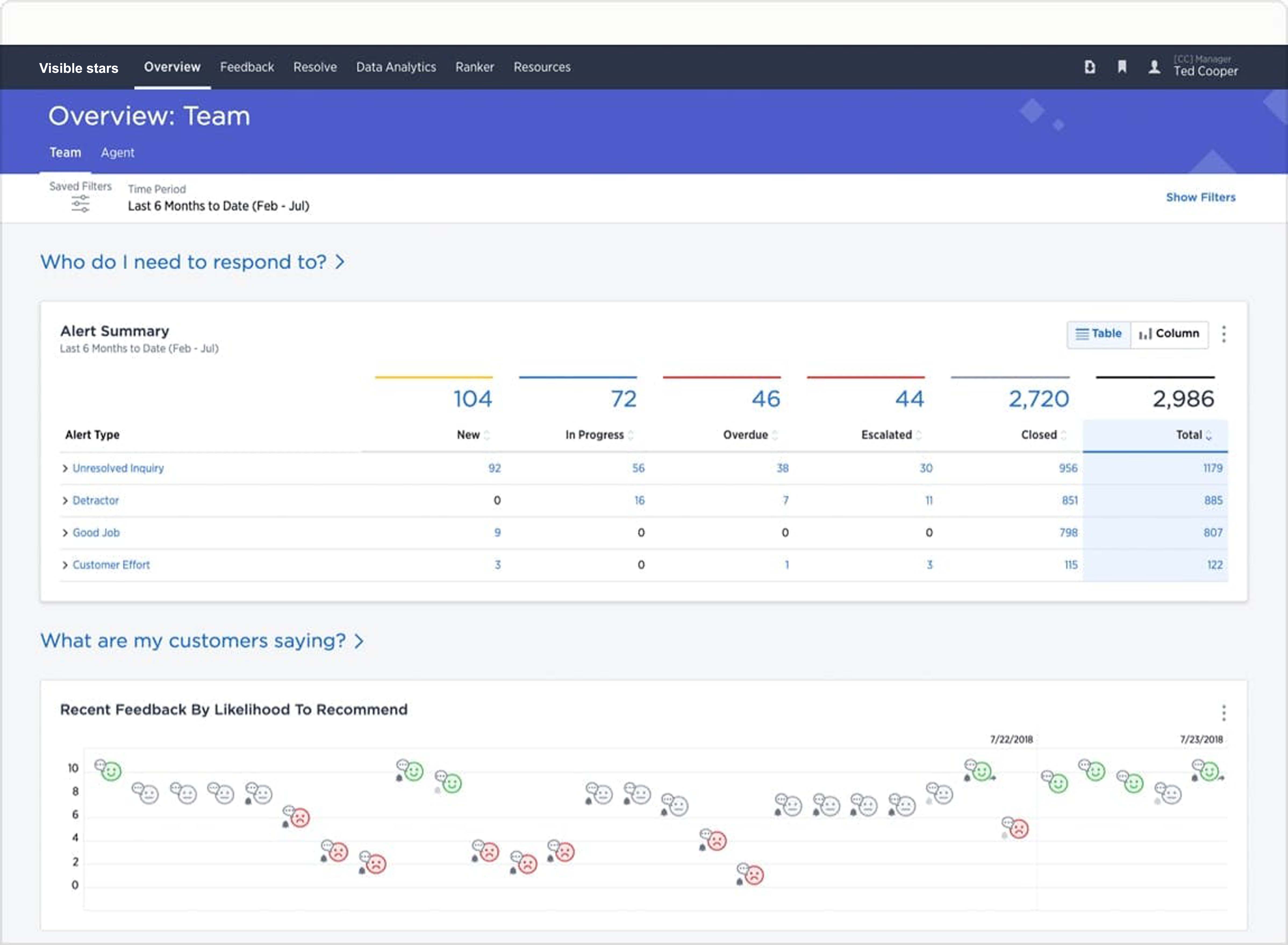
- Alert the appropriate caregiver(s) and prompt them to take action in real-time. Enable leaders to get visibility across the organization to identify and prioritize investment opportunities and drive change innovation
- Increase caregiver morale by providing real-time positive acknowledgement
Healthcare & Insurance
World-class experience management for Providers and Payers
Personalized and predictive insights and action recommendations strengthen relationships in a rapidly evolving industry
Healthcare & Insurance
World-class experience management for Providers and Payers
Personalized and predictive insights and action recommendations strengthen relationships in a rapidly evolving industry
Healthcare
Pre-built solutions for optimizing patient, member, and client experiences to achieve superior outcomes
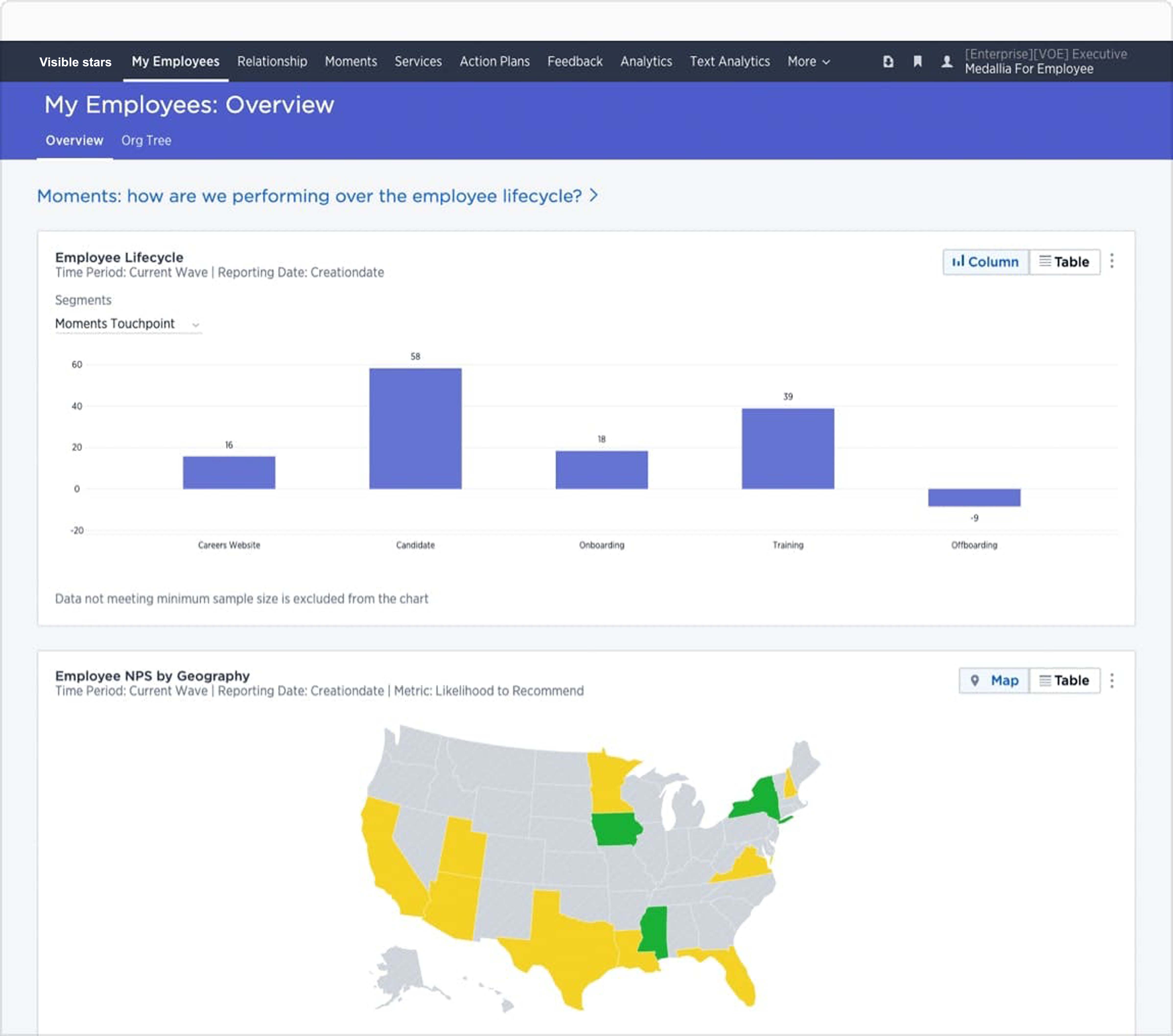
Visible Stars enables healthcare companies to exceed customer expectations, motivate and engage staff, and innovate to drive brand and customer loyalty. We help providers, payers, and suppliers capture feedback, integrate experience data with operational data - from CRM and EHR systems - and turn them into actionable insights for everyone, ranging from frontline and support staff to clinicians and executives.
FOR PROVIDERS
Capture experience signals wherever patients and caregivers are, integrate with operational data, and deliver insights that enable action in real-time.
Patient Experience for Providers
FOR PAYERS
Enhance member, employer and broker experiences to grow market share, reduce operational expenses, and improve product offerings.
Member Experience for Payers
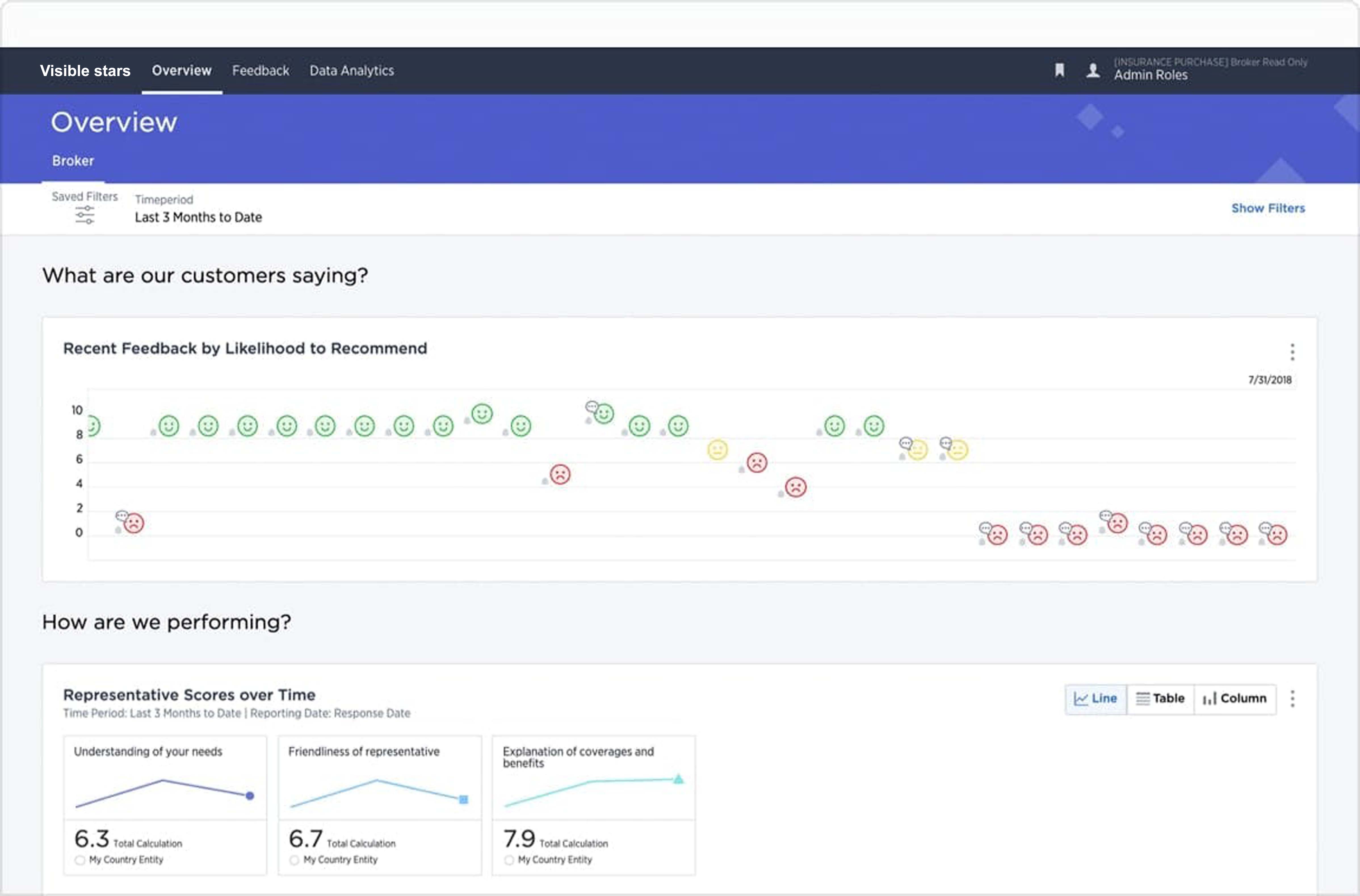
- Capture, analyze and act on experience signals to improve the member experience and broker behavior. Make it easy for members to engage with their health plan and increase satisfaction, retention and share of wallet
- Combine experience signals and operational data to provide rich context of how, when, and where to drive operational and product improvements
- Systematically understand key drivers of both positive and negative experiences. Prioritize process improvements in order to reduce operating expenditures
Recognition and Awards

Visible Stars is included in the 2019 KLAS Patient Engagement Ecosystem Report.
Visible Stars’s capabilities have been validated in the following areas:
- Knowing the Patient
- Patient Empowerment
- Patient Experience
- Types of HIT Solutions Typically Used for Partnership

Customer Quote from 2019 KLAS Patient Engagement Ecosystem Report
“Visible Stars Experience Cloud is a management system for customer feedback, and we actually have some other systems in play as well. We are moving away from the other systems because we like Visible Stars’s platform quite a bit. We get feedback more quickly with Visible Stars's software. The other piece Visible Stars offers that we love is the reporting, which is great. We can recover service in real time. We have the system installed to a degree on a mobile app, so when feedback comes in, we can actually see that on our phones instantaneously. We don’t have the system set up to see patient information right now, but that can be done too.”
– Director of Customer Experience
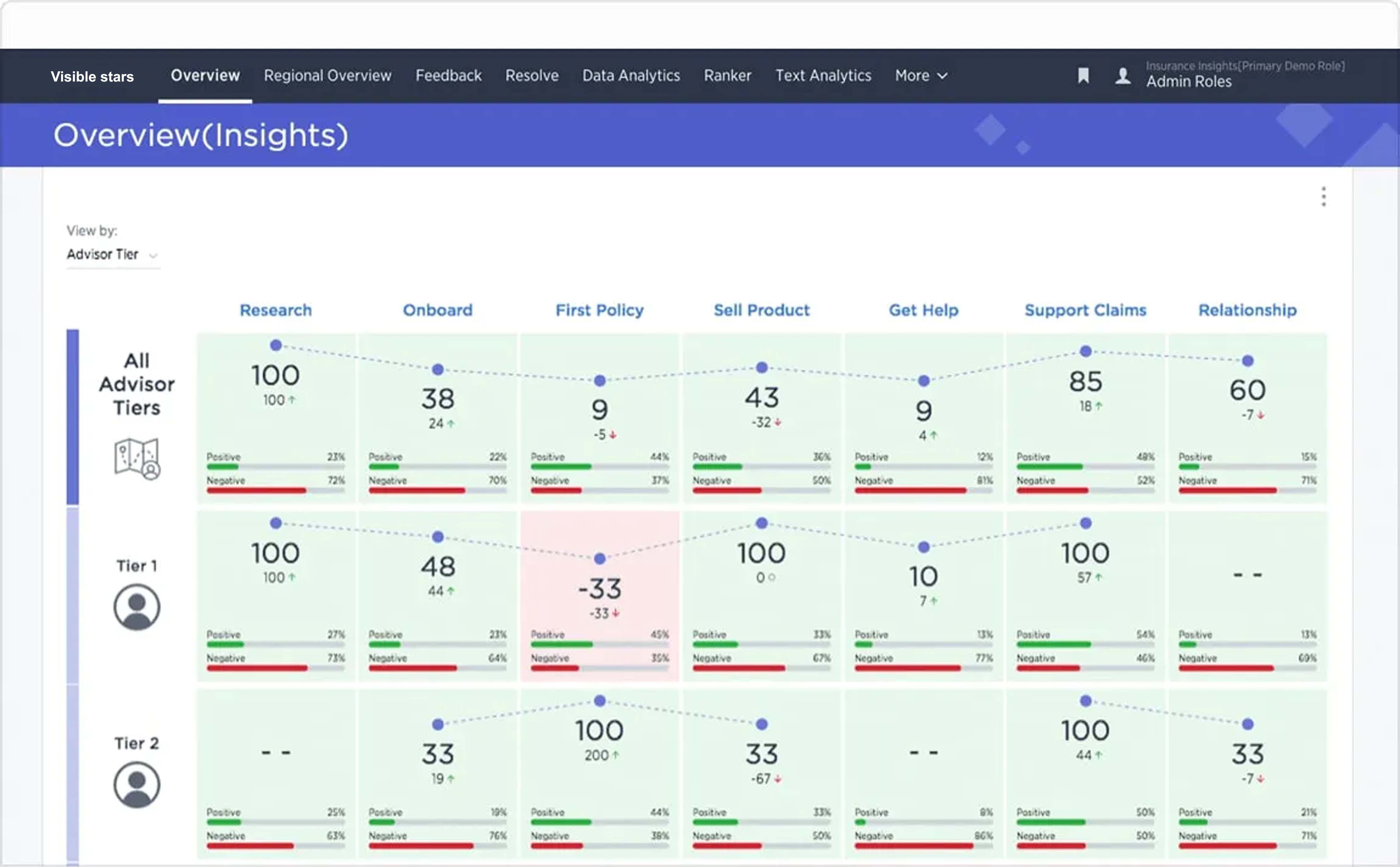
Insurance


Minimize risk by understanding and anticipating the needs of policyholders, agents, and brokers.
In an industry that is so dependent on trust, every experience plays a critical role in building or breaking it. Visible Stars helps insurers orchestrate every customer, employee, and agent journey to predict and prioritize the actions needed to deliver experiences that contribute to successful, healthy, long-term relationships.
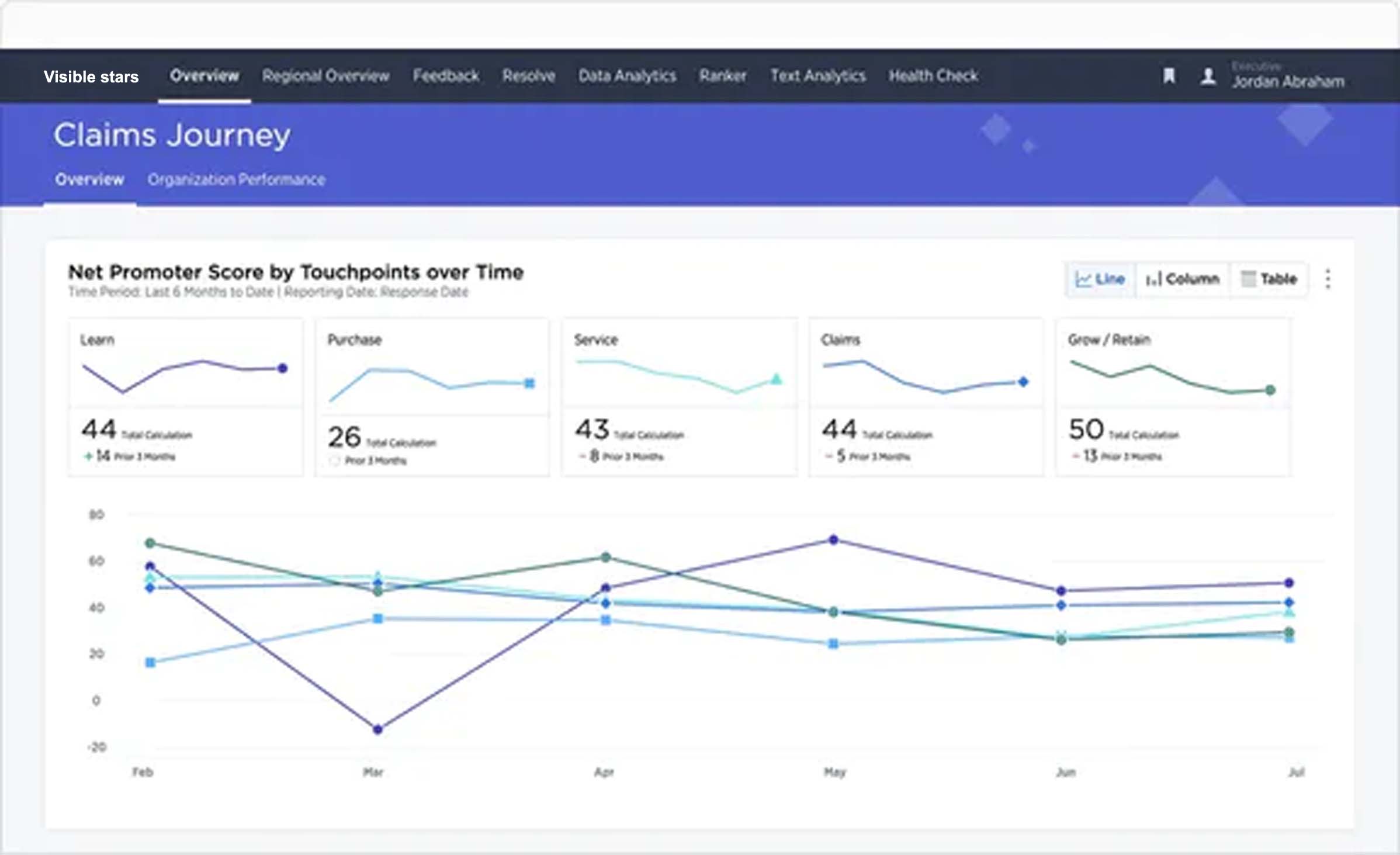
PROPERTY & CASUALTY
Turn claimants into brand ambassadors

Claimants with positive experiences are more likely to renew and recommend their insurer. Prioritize the necessary actions needed to delight every customer, employee and agent
- Capture customer signals across the entire claims journey to identify opportunities to improve policyholder experience to drive issuance, on-going satisfaction and policy renewal
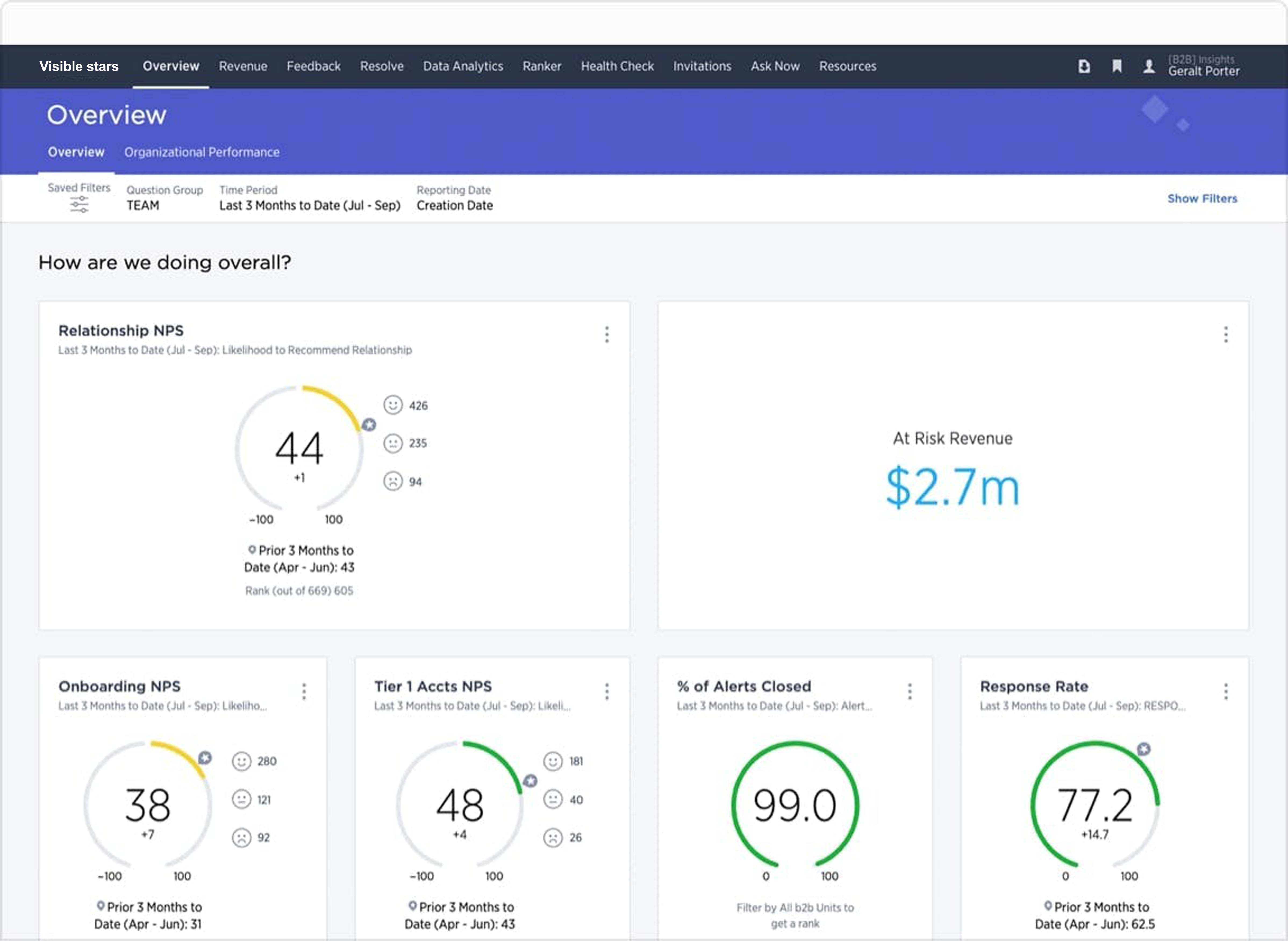
- Accelerate frontline productivity by giving every claims adjuster, underwriter, service representative, and agent visibility into their performance from the customer’s perspective and the insights needed to improve
- Minimize policyholder churn by leveraging 360-views of account health and addressing early warning signals and proven client retention strategies
LIFE & ANNUITY
Frictionless experiences at scale

Use customer, employee and broker insights to predict and prioritize the actions that will make every experience easy and efficient
- Leverage predictive models to identify customer pain points and prioritize ways to improve experiences from application to issue
- Create opportunities to cross-sell additional financial service solutions by ensuring that every customer experience is the highest quality
- Understand employee and advisor experiences to optimize training programs that improve performance while deepening partner relationships
Enterprise Grade Security, Privacy, Accessibility
Our Security and Privacy controls meet the high standards of public agencies and highly regulated markets. We offer solutions that meet the accessibility standards of WCAG 2.0 AA and Section 508 of the Americans with Disabilities Act, as applicable.

Brochure
The “Why” Behind the NPS® Score
Net Promoter Score (NPS)® is a powerful tool in gauging customer loyalty and, by extension, company health. Learn how you can use it in your own CEM program.